CPAP Support and Education
- Educators are still taking consultations with patients either after consultations with Dr Scott or for pre-arranged visits.
- All consultations are being triaged into urgent, semi-urgent, and routine.
- When possible, the preferred payment method is contactless via PayPass. We prefer cash not to be used. The EFTPOS terminal will be wiped down after each use.
- For Patients in our local geographical area we offer Home CPAP Service. It may be an option for one of our trained CPAP educators can visit you in the comfort and safety of your home.
CPAP Consultations
- Routine Consultation: upon receipt of an emailed request, a CPAP educator will contact you by telephone to provide support. All equipment requirements, such as masks, parts and filters, will be available via post.
- Semi-urgent and Urgent Consultations: under certain circumstance an in-person consultation may be required to solve issues with CPAP therapy. Upon receipt of an email enquiry, our CPAP educators will contact you to determine if this is required.
CPAP In-clinic Cleaning Schedule
- All staff have received specialist COVID-19 Infection Control training and are certified according to Queensland Health Guidelines.
- Educators will be wiping over all surfaces (benches and couches) in between patients. Due to this, there may be slightly longer waiting times to see an educator. They will also adhere to the recommended Personal Protective Equipment (PPE).
- Where possible, social distancing measures will be observed. Due to the nature of the consultations, social distancing is not always applicable (eg: mask fittings, etc) but it is maintained when possible.
- CPAP equipment undergoes strict disinfection protocols with machines and mask parts:
- Machines are wiped over with hospital grade sanitizer solution with filters being changed regularly
- Mask parts are soaked in hospital grade sanitizer solution before going through our standard hospital grade SMEG wash which utilizes a hypochlorite chemical at 80°C for 10 minutes, as per the Queensland Health Infection Control Guidelines.
CPAP Therapy – What to do at home?
- People with Obstructive Sleep Apnoea (OSA) should continue to use their CPAP at home as normal.
- Currently, there is no evidence that CPAP usage makes you more susceptible to catching COVID-19 or makes you more unwell if you have it already.
- It is unknown whether CPAP usage while having COVID-19 increases the likelihood of the virus spreading. Self-isolation should be occurring regardless if you have the virus.
- If you have a respiratory infection, CPAP usage can become difficult. It is recommended you continue to use the device until it becomes too uncomfortable to do so. Once the symptoms diminish, it is strongly recommended to recommence therapy.
- Maintaining your routine cleaning of the device is important. This includes the daily wipe over of equipment and humidifier tank being emptied and refilled. Weekly cleaning is to proceed as normal including washing all parts and allowing ample time to dry (out of direct sunlight) before using again at night.
- Please be sure to take extra care of the equipment as supplies may be temporarily unavailable. If new equipment is required, delivery of replacement parts to your home address can be organized.



Please click on the mask below for a video about correct fitting
CPAP Cleaning Checklist
DAILY
Mask
- Rinse the mask cushion off with water and wipe with a damp fabric cloth to remove saliva or excess skin oils.
Humidifier
- Empty the water chamber in the morning and fill the chamber with water at night.
WEEKLY
Mask and Tubing
- Clean the machine tubing, humidifier chamber and all mask parts (head straps, mouth and nasal cushion and pieces) in warm soapy water (use a mild detergent), soak for 15 minutes then rinse thoroughly with clean water.
- Hang the equipment up to dry out of direct sunlight.
- Try and do your weekly clean in the morning so it’s dry by night.
MONTHLY
Filters
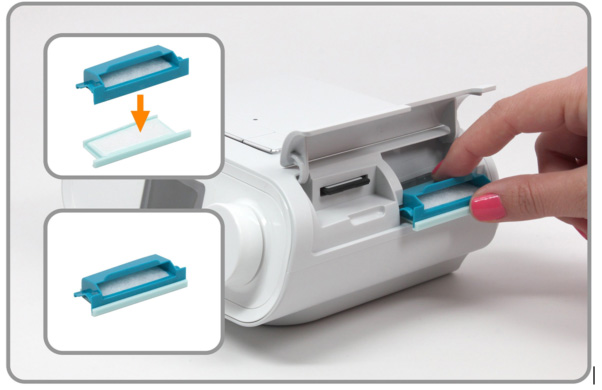
- Inspect the dark blue pollen filter monthly, rinse with water to remove and leave to dry (do not scrub or use soaps).
- If you use the light blue fine filter, please remove when washing as this component cannot get wet.
- Replace the light blue fine filter underneath the pollen filter every month. Do not get wet and always use in conjunction with the pollen filter. If you run out, you can use your device with the single pollen filter in its own.
How do I change my filters?
Humidifier
- Inspect for lime scale build up. If present soak the chamber in water equal parts water and vinegar for 30 minutes and then scrub with a soft toothbrush. Rinse thoroughly with clean water.
YEARLY
Mask
- Parts of your mask may require replacement so check the elasticity of straps, look for mould in the nasal or mouth cushions, or any tears/holes in the silicon pieces.
Data
- You should have your data checked every 6-12 months (this will be completed during your follow up appointments).
Adjusting DreamStation Humidity

The bottom right number is the humidity level.
This comfort feature controls the level of humidity in the air that comes out of your CPAP tubing and into your mask.
It is designed to prevent dryness of the nose and mouth.
If you are experiencing a dry nose or throat increase the level of humidity.
If you are experiencing condensation in your mask decrease the level of humidity.
- Turn the dial to highlight humidity (turns orange)
- Press the centre of the dial (turns grey)
- Move the dial left or right, the scale range is 0 to 5, 0 is the lowest, 5 is the highest
- Press the centre of the dial to “set” the required level
Adjusting DreamStation Heated Tubing

The top right number is the heated tubing level.
This comfort feature controls the temperature that comes out of the air through your CPAP tubing and into your mask.
If the air is too hot then turn down the amount of heat
If the air is too cold then turn up the amount of heat
- Turn the dial to highlight heated tubing (turns orange)
- Press the centre of the dial (turns grey)
- Move the dial left or right, the scale range is 0 to 5, 0 is the lowest, 5 is the highest
- Press the centre of the dial to “set” the required level
How to manage active Rhinosinusitis
Chronic sinusitis and acute sinusitis have similar signs and symptoms, but acute sinusitis is a temporary infection of the sinuses often associated with a common cold, allergy or generalised nasal irritation. Acute sinusitis, also called acute rhinosinusitis, is a short-term inflammation of the membranes that line your nose and surrounding sinuses. This impedes your ability to drain mucus from your nose and sinuses. Acute sinusitis is most commonly due to a cold causing viral infection. However, it can be due to non-infectious causes as well.
Symptoms of active rhinosinusitis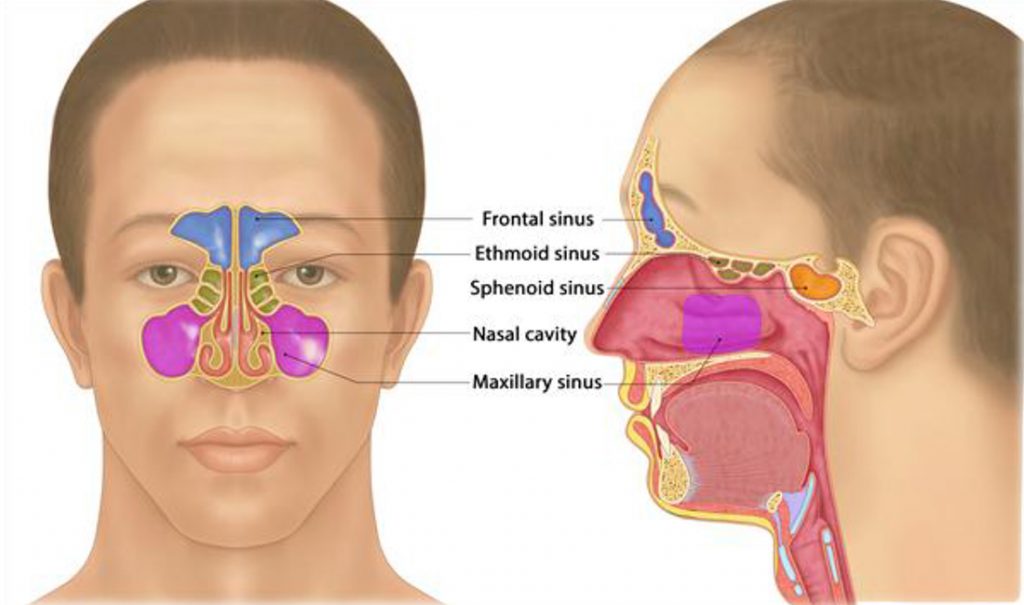
- Nasal congestion
- Sore throat
- Cough, may be worse at night
- Drainage of mucus in the back of your throat (post-nasal drip)
- Headache
- Pain pressure or tenderness behind the eyes, cheeks or forehead
- Yellow or green mucus discharge from nose
Management of active Inflammatory Rhinosinusitis
Some cases of acute rhinosinusitis can be treated at home:
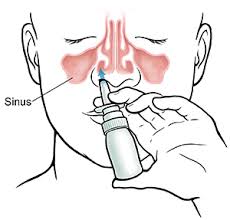
- Saline nasal sprays: use several times a day to rinse and clear nasal passages.
- Over-the-counter (OTC) nasal corticoid spray: sprays such as Nasonex, Rhinocort, Flixonase and Beconase can reduce intranasal inflammation
Some cases of rhinosinusitis may be more severe and infectious. Please consult your doctor if you have experienced symptoms for more than 12 weeks. Your doctor may prescribe antibiotic therapy or other medications, if clinically indicated.
How to use a nasal spray correctly: CLICK HERE TO VIEW VIDEO