Lung Cancer
LUNG CANCER STATISTICS
- Lung cancer is the leading cause of death due to cancer in Australia.
- Lung cancer is the 3rd leading cause of all deaths in Australia
- Lung cancer is the 5th most common cancer in Australia.
- More than 9,100 Australians are diagnosed with lung cancer each year.
- More than 7,600 Australians die from lung cancer each year – that is almost 20 people per day, every day of the year.
- 40% of those diagnosed with lung cancer have either never smoked or have long since kicked the habit.
Ref: Australian Lung Foundation
WHAT IS LUNG CANCER?
Lung cancer is an abnormality in the cells of the lung and usually starts in the lining of an airway. There are different types of lung cancer, which are classified according to the type of cell affected.
The three types are:
- small cell lung cancer
- non-small cell lung cancer.
- Mesothelioma (less common)
SMALL CELL LUNG CANCER (SCLC)
- Makes up around 15% of lung cancers.
- Strongly linked with cigarette smoking.
- Tends to start in the middle of the lungs.
- Surgery is not often used for this type of tumour — it’s usually treated with drugs (chemotherapy) combined with radiotherapy.
- Named for the way cells look under a microscope.
- Types include small cell carcinoma (“oat cell cancer”), mixed small cell/large cell carcinoma and combined cell carcinoma.
NON-SMALL CELL LUNG CANCER
- Makes up around 75-80% of lung cancers.
- Mainly affects the cells that line the tubes into the lungs (main bronchi) and smaller airways.
- If a non-small cell lung cancer is confined to a part of the lung, it might be surgically removed.
- If non-small cell lung cancer is not suitable for surgery other treatments may be necessary.
- Sometimes spreads into the chest wall and lymph nodes.
- Includes squamous cell carcinoma, adenocarcinoma, large cell carcinoma and bronchiolo-alveolar cell carcinoma.
MESOTHELIOMA
Malignant mesothelioma is cancer of the cells of the pleural membrane around the lungs.
- This is rare, but Australia has the highest incidence in the world (40 cases/million people).
- Strongly linked to asbestos exposure.
- Sometimes 25-50 years pass between asbestos exposure and development of the disease.
*Ref: Cancer Council
CAUSES OF LUNG CANCER
SMOKING
Smoking causes up to 90% of lung cancers and about 1/10 of people who smoke develop lung cancer. Lung cancer is not usually seen in people under 40 years old, but risk increases significantly for people aged 50 and older.
If a person starts smoking when they are young, they are at a higher risk of getting lung cancer.
PASSIVE SMOKING
Passive (secondhand) tobacco smoke can cause lung cancer, but the risks are less than if you smoke.
WORK-RELATED RISKS
Exposure to the following is associated with an increased risk of lung cancer:
- asbestos
- processing of steel, nickel, chrome and coal gas
- radiation. Miners may be exposed to radiation by breathing air contaminated with radon gas.
SYMPTOMS OF LUNG CANCER
Common symptoms of lung cancer include:
- Bloody sputum (phlegm)
- Chest pain
- Cough
- Loss of appetite
- Shortness of breath
- Weight loss
- Wheezing
Other symptoms that may occur with this disease:
- Facial swelling
- Fever
- Hoarseness or changing voice
- Swallowing difficulty
- Weakness
HOW LUNG CANCER IS DIAGNOSED
PHYSICAL EXAMINATION
Your doctor will first ask you about your past and current health, smoking and work history, and do a physical examination. They may suggest that you have some of the following tests.
Chest x-ray – An x-ray of the chest can find cancers as small as 1 cm.
Sputum cytology – testing your phlegm for abnormal cells
Bronchoscopy – a telescope is inserted into your nose/mouth to take a sample of tissue for analysis.
Fine-needle aspiration – This allows the doctor to take a sample of tissue from a lump that cannot be sampled using bronchoscopy.
Mediastinoscopy – In this test, the doctor is able to look at lymph nodes in the centre of the chest, to see if they are affected by cancer. The procedure is similar to bronchoscopy, but the tube is inserted through a cut in the neck and fed down to the lymph nodes around the windpipe.
Video-assisted thoracoscopic surgery – This test allows the doctor to see inside the chest and take tissue samples if necessary. Instruments are inserted into the chest cavity through small cuts in the skin.
Computerised tomography (CT) scan – A CT scan is a type of x-ray that gives a cross-sectional picture of organs and other structures (including any tumours) in your body. It can be used to see smaller cancers than those found by x-rays. It can also show if lymph nodes are enlarged or if the cancer has spread to other organs.
STAGES OF LUNG CANCER
The above tests will help the doctor determine whether you have cancer. They will also show where the primary cancer is and whether the cancer cells have spread to other parts of your body. This helps your doctors ‘stage’ the disease.
‘Stage’ describes the extent of the cancer in your body. It helps show which treatment is needed. It is also a guide to prognosis.
STAGING SMALL CELL LUNG CANCER
Small cell lung cancer has often spread outside the chest when it is diagnosed.
It is staged in two ways:
- Limited disease — when the tumour can be detected in only one lung and nearby lymph glands.
- Extensive disease — other cases.
STAGING NON-SMALL CELL LUNG CANCER
Staging non-small cell lung cancer is more complex. The following is a simplified guide to staging this condition:
- Stage 1
Tumours are only in one lobe of the lung. - Stage 2
A tumour in the lung with limited spread to nearby lymph nodes, or a tumour that has grown into the chest wall. - Stage 3A
Tumours have spread to lymph nodes in the centre of the chest (the mediastinum). - Stage 3B
Tumours have spread more extensively to lymph nodes in the mediastinum, or there is a collection of fluid in the pleural space around the lung, or there are tumours in more than one lobe. - Stage 4
The cancer cells have spread to distant parts of the body. Lung cancer sometimes spreads to the bones, the liver and to the adrenal glands (the glands that sit on top of the kidneys and regulate stress response).
Ref: Cancer Council Australia
TREATMENT OF LUNG CANCER
SMALL CELL LUNG CANCER
- Chemotherapy.
- Radiotherapy – usually for people with limited disease. Sometimes radiotherapy is also given to the brain to prevent the cancer spreading.
NON-SMALL CELL LUNG CANCER
The main treatments for this type of lung cancer are:
- surgery
- radiotherapy
- chemotherapy
The choice of treatment will depend on the stage of your cancer, your general health, whether you are fit enough to have an anaesthetic and operation, and whether your lungs are working well enough.
The aim of treatment is to keep you as well and symptom-free as possible, even if your cancer cannot be cured.
HOW CAN LUNG CANCER BE PREVENTED?
DO NOT SMOKE!
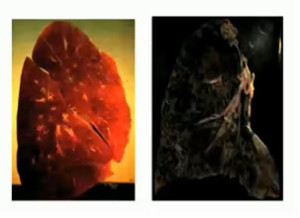
This is the main message for lung cancer prevention so we’ll repeat it – do not smoke! This is what it does to your lungs:
Comparison of a Normal Lung (left) versus a Smoker’s lung (right)
Avoiding smoking will not only significantly reduce the risk of lung cancer, but also the risk of a number of other cancers and chronic diseases.
There are a number of ways to help people quit smoking, including nicotine replacement therapy, courses and pharmacological aids. Support from family and friends can make a big difference, as can sound advice from a health professional or the Quitline. Most smokers prefer to quit on their own, with 90 per cent of smokers successfully quitting without aids. However, many smokers may make several attempts to quit before succeeding. The key is to have a good plan, keep trying and to learn from previous attempts.
For more advice on quitting, call the Quitline on 13 18 48 or talk to your GP.