30 Aug The COPD-X Plan
Introduction: Chronic obstructive pulmonary disease (COPD) is characterised by persistent respiratory symptoms and chronic airflow limitation, and is associated with exacerbations and comorbidities. Advances in the management of COPD are updated quarterly in the national COPD guidelines, the COPD-X plan, published by Lung Foundation Australia in conjunction with the Thoracic Society of Australia and New Zealand and available at http://copdx.org.au.
To read the most current updates click here: https://copdx.org.au/wp-content/uploads/2018/08/Summary-of-Changes-V2-54-June-2018-FINAL.pdf
Main recommendations:
- Spirometry detects persistent airflow limitation (post-bronchodilator FEV1/FVC < 0.7) and must be used to confirm the diagnosis.
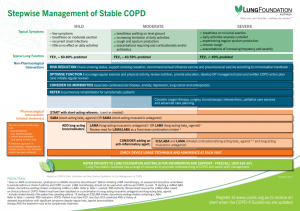
- Non-pharmacological and pharmacological therapies should be considered as they optimise function (ie, improve symptoms and quality of life) and prevent deterioration (ie, prevent exacerbations and reduce decline).
- Pulmonary rehabilitation and regular exercise are highly beneficial and should be provided to all symptomatic COPD patients.
- Short- and long-acting inhaled bronchodilators and, in more severe disease, anti-inflammatory agents (inhaled corticosteroids) should be considered in a stepwise approach.
- Given the wide range of inhaler devices available, inhaler technique and adherence should be checked regularly.
- Smoking cessation is essential, and influenza and pneumococcal vaccinations reduce the risk of exacerbations.
- A plan of care should be developed with the multidisciplinary team. COPD action plans reduce hospitalisations and are recommended as part of COPD self-management.
- Exacerbations should be managed promptly with bronchodilators, corticosteroids and antibiotics as appropriate to prevent hospital admission and delay COPD progression.
- Comorbidities of COPD require identification and appropriate management.
- Supportive, palliative and end-of-life care are beneficial for patients with advanced disease.
- Education of patients, carers and clinicians, and a strong partnership between primary and tertiary care, facilitate evidence-based management of COPD.
Changes in management as result of the guideline: Spirometry remains the gold standard for diagnosing airflow obstruction and COPD. Non-pharmacological and pharmacological treatment should be used in a stepwise fashion to control symptoms and reduce exacerbation risk.
C CONFIRM DIAGNOSIS
Clinical features, Spirometry, Investigations, Severity.
O OPTIMISE FUNCTION
Non-pharmacological strategies, Pharmaceutical strategies (Bronchodilators; Anti-inflammatory agents), Inhaler technique, Comorbidities, Lung volume reduction.
P PREVENT DETERIORATION
Smoking cessation, Vaccinations, Long term oxygen therapy.
D DEVELOP A PLAN OF CARE
Chronic disease management and self-management, Multidisciplinary team, COPD action plan.
X MANAGE EXACERBATIONS
Pharmacological management of exacerbations, Discharge planning, Oxygen therapy and non-invasive ventilation, Post-discharge pulmonary rehabilitation.