07 Oct Thyroid disorders and sleep
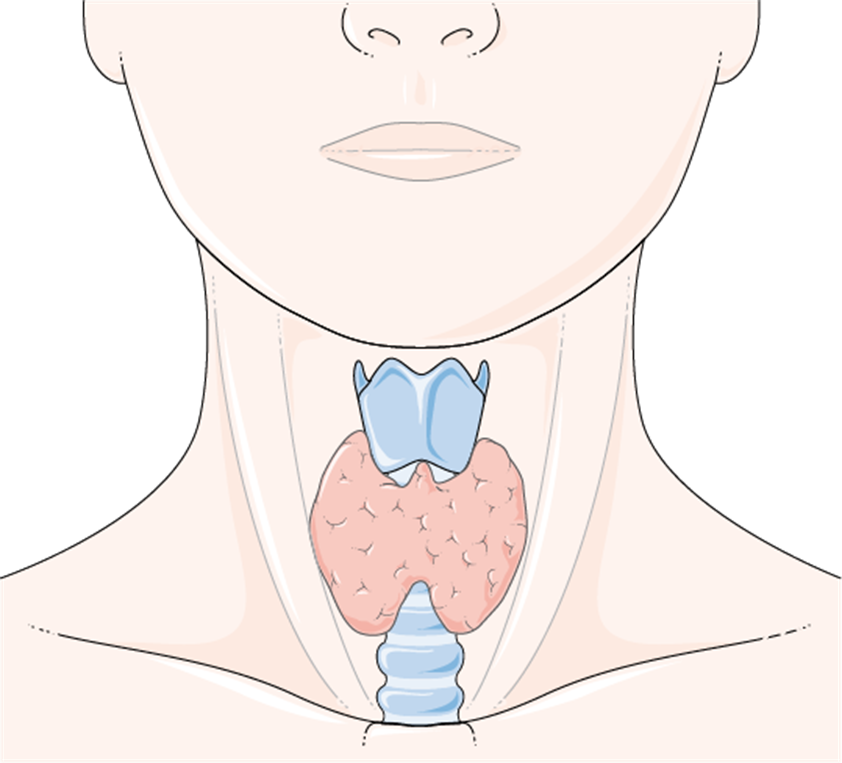
The thyroid
The thyroid has numerous functions such as the regulation of body temperature, digestion, heart rate and respiratory function. The thyroid regulates respiratory function via the hormone thyroxine. There are two main types of thyroid dysfunction, they are hypothyroidism and hyperthyroidism. Hypothyroidism is the result of low levels of thyroid hormones (Triiodothyronine [T3] and thyroxine [T4]). Hyperthyroidism is the opposite of hypothyroidism; it is the excess production of thyroid hormones (Triiodothyronine [T3] and thyroxine [T4]), as well as, low or supressed levels of thyroid stimulating hormone (TSH).
Thyroid disorders and Obstructive Sleep Apnoea (OSA)
Obstructive sleep apnoea (OSA) is the repeated collapse or narrowing of the upper airway causing oxygen desaturations or cortical arousals. This leads to fragmented sleep, cardiovascular damage and poor mental health.
The link between thyroid disorders and OSA has been widely studied but there is no clear consensus with regards to the pathophysiological way in which they interrelate. Various studies conducted over the decades have hypothesised that thyroid disorders relate to OSA in the following ways.
Hypothyroidism impacts respiratory function via the weakening of the respiratory muscles, a reduction in lung capacity and partial upper airway obstruction from oedema and diaphragmatic dysfunction.
The impact of hyperthyroidism on respiratory function in terms of OSA is not well studied, however dyspnoea is related to cardiac disorders (Palpitations, peripheral oedema and congestive heart failure)
Comorbidities and links that are related to OSA and thyroid disorders include; obesity, thyroid size (hypothyroidism. Increased thyroid size increases airway susceptibility to obstruction), hypertension, smoking.
Thyroid disorders and Insomnia
Insomnia is defined as difficulty falling asleep at least three times a week for three or more weeks. It has been suggested in studies that hyperthyroidism is linked to several factors of sleep dysfunction including: prolonged sleep onset, difficulty maintaining sleep and excessive daytime sleepiness. Furthermore, hyperthyroidism has been found to worsen conditions such as anxiety and depression further impairing sleep and increasing the risk of insomnia.
No direct connection has been found between insomnia and hypothyroidism. However, symptoms of hypothyroidism such as intolerance to coldness and increased anxiety can increase the risk of insomnia.
Thyroid disorders and restless legs syndrome (RLS)
RLS is musculoskeletal disorder defined as an unpleasant sensation and the urge to move the lower limbs (Legs) in the evening or at night while attempting to sleep. Symptoms typically disappear upon movement. It has been hypothesized that RLS occurs due to iron deficiency in the central nervous system impacting the dopaminergic pathways.
While thyroid disorders and RLS is not well researched it is hypothesized that thyroid disorders exacerbate RLS symptoms. Furthermore, Pereira et al (2010) hypothesized that insufficient dopamine related to the pathophysiology of RLS inhibited TSH release. This in turn reduces the perceptual threshold of sensory stimuli in the lower limbs. However, this has not been studied at a clinical level.
References:
Ertek, S., & Cicero, A. F. (2013). State of the art paper Hyperthyroidism and cardiovascular complications: a narrative review on the basis of pathophysiology. Archives of Medical Science, 5, 944–952. https://doi.org/10.5114/aoms.2013.38685
File:Glands – Normal thyroid — Smart-Servier.png. (2023, November 16). Wikimedia Commons. Retrieved October 7, 2025, from https://commons.wikimedia.org/w/index.php?title=File:Glands_-_Normal_thyroid_–_Smart-Servier.png&oldid=822286585.
Green, M. E., Bernet, V., & Cheung, J. (2021a). Thyroid dysfunction and sleep disorders. Frontiers in Endocrinology, 12. https://doi.org/10.3389/fendo.2021.725829
Lencu, C., Alexescu, T., Petrulea, M., & Lencu, M. (2016). RESPIRATORY MANIFESTATIONS IN ENDOCRINE DISEASES. Medicine and Pharmacy Reports, 89(4), 459–463. https://doi.org/10.15386/cjmed-671
Mathew, P., Kaur, J., & Rawla, P. (2023, March 19). Hyperthyroidism. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537053/
McNamara S, Spurling BC, Bollu PC. Chronic Insomnia. [Updated 2025 Mar 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526136/
Patil, N., Rehman, A., Anastasopoulou, C., & Jialal, I. (2024, February 18). Hypothyroidism. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519536/
Pelizzo, G., Calcaterra, V., Baldassarre, P., Marinaro, M., Taranto, S., Ceresola, M., Capelo, G., Gazzola, C., & Zuccotti, G. (2024). The impact of hormones on lung development and function: an overlooked aspect to consider from early childhood. Frontiers in Endocrinology, 15. https://doi.org/10.3389/fendo.2024.1425149
Shi, Y., Cao, Z., Xie, Y., Yuan, Y., Chen, X., Su, Y., Niu, X., Liu, H., Yin, L., Zhao, B., Liu, H., She, N., Feng, Y., Wang, Z., Zhang, Y., Ma, L., & Ren, X. (2023). Association between obstructive sleep apnea and thyroid function: A 10-year retrospective study. Sleep Medicine, 103, 106–115. https://doi.org/10.1016/j.sleep.2023.01.027
Slowik, J. M., Sankari, A., & Collen, J. F. (2025, March 4). Obstructive sleep apnea. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459252/
Suwała, S., Rzeszuto, J., Glonek, R., Krintus, M., & Junik, R. (2022). Is restless legs syndrome de facto thyroid disease? Biomedicines, 10(10), 2502. https://doi.org/10.3390/biomedicines10102502

