04 Dec Medicating Insomnia by Targeting Underlying Neurological Deficiencies
Posted at 15:24h
in Blog
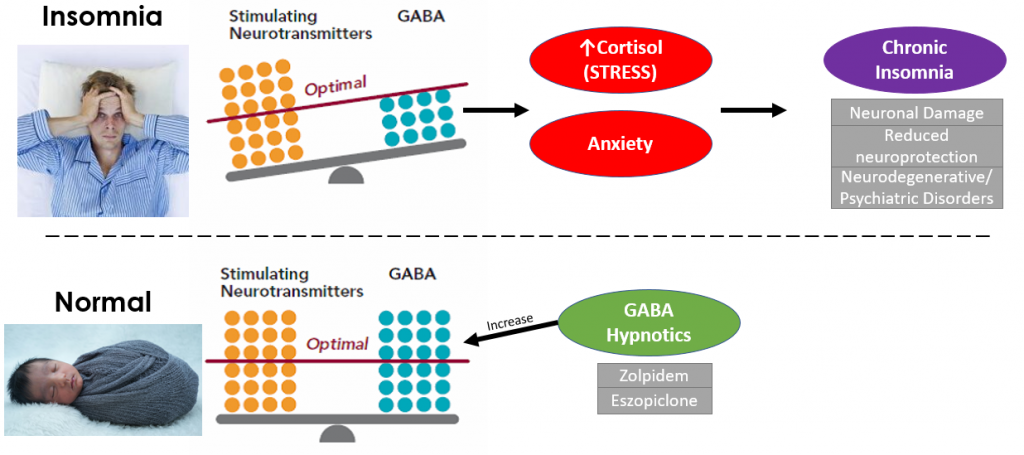
Insomnia is more than a few bad nights. Modern research shows it reflects deeper changes in the brain’s chemical balance — and that the right treatments can begin restoring both sleep and brain health.
A new study by Kumar and other researchers offers an important clue. Participants treated with either the hypnotic medications zolpidem or clobazam for 12 weeks not only slept longer and better, they also showed increased levels of BDNF, a key brain-growth molecule. This matters because BDNF (Brain-Derived Neurotrophic Factor) supports learning, memory, emotional stability, and the brain’s ability to repair itself. Low BDNF has repeatedly been linked to chronic insomnia, anxiety, depression and long-term cognitive decline. Only in the last few years has the low levels of BDNF revealed itself as a key underlying target to treat chronic insomnia.
Why insomnia starts: the glutamate–GABA imbalance
Your brain operates on a delicate balance between “go” signals (primarily glutamate) and “slow-down” signals (GABA).
In insomnia, this balance is tilted:
In insomnia, this balance is tilted:
- Too much glutamate → racing thoughts, emotional overreactivity, lying awake even when exhausted
- Too little GABA → the brain cannot “switch off” at night
- Over time, this hyperarousal reduces BDNF and stresses neural circuits
This is why insomnia often feels like the nervous system is stuck in “high alert,” even when you desperately want to rest.
The real long-term risk
Chronic insomnia increases vulnerability to depression, anxiety, and age-related cognitive decline. The likely path: years of night-time overarousal + low BDNF slowly strain the brain’s resilience and has been found to heighten your chance of developing neurodegenerative and psychiatric disorders. Early and effective treatment can help break this cycle.
Popular Anti-Insomnia Medications
(Evidence-based medications with behavioural therapy isn’t enough)
- Orexin Receptor Antagonists — Suvorexant, Lemborexant
These switch off the brain’s wake-promoting orexin system.
Best for: staying asleep. Use if you wake up frequently throughout the night.
Low risk of dependence and minimal hangover.
Best for: staying asleep. Use if you wake up frequently throughout the night.
Low risk of dependence and minimal hangover.
- Z-drugs — Zolpidem, Eszopiclone (Short-Term Use)
Fast and effective for getting to sleep quicker.
The recent study mentioned earlier highlights zolpidem’s potential to restore BDNF, hinting at a biological benefit beyond sedation.
Must be used short term and under supervision.
The recent study mentioned earlier highlights zolpidem’s potential to restore BDNF, hinting at a biological benefit beyond sedation.
Must be used short term and under supervision.
- Melatonin & Melatonin-Receptor Agonists (Ramelteon)
Help realign the sleep–wake rhythm.
Very safe, non-habit forming.
Very safe, non-habit forming.
Current Medications that Should be Avoided
- Long-Term Benzodiazepines (e.g., Temazepam, Diazepam)
High risk of dependence, tolerance, memory problems, and withdrawal.
Not suitable for chronic insomnia.
Not suitable for chronic insomnia.
- Sedating Antihistamines (e.g., Diphenhydramine “Nighttime” Products)
Cause grogginess, confusion, and anticholinergic side effects — especially risky for older adults. Common over-the-counter anti-insomnia medication.
Not recommended for long-term sleep.
Not recommended for long-term sleep.
- Off-Label Antipsychotics (e.g., Quetiapine)
Increasingly given for sleep but linked to weight gain, metabolic issues, daytime sedation, and serious long-term risks.
When to Seek Specialist Help
If your sleep has been poor for more than three months, or if you’re noticing changes in mood, concentration, or daytime functioning, a sleep specialist can assess the underlying causes and create a safe, effective plan — usually starting with cognitive behavioural therapy and adding medication only when beneficial.
References
Kumar V, Halder S, Srivastava S, Kar R, Jain S, Almeida EA. Sleep, BDNF, and beyond: A comparative study of zolpidem and clobazam in insomnia treatment. Sleep Med. 2025 Nov 1;137:106893. doi: 10.1016/j.sleep.2025.106893. Epub ahead of print. PMID: 41197179.
Berry, R. B., Wagner, M. H., & Ryals, S. M. (2025). Fundamentals of sleep medicine (Second edition.). Elsevier.

