
03 Oct THE IMPACT OF WEIGHT REDUCTION IN THE PREVENTION OF THE PROGRESSION OF OBSTRUCTIVE SLEEP APNEA
Numerous studies have attributed the pathophysiology of lipid metabolism disorders in sleep apnoea mainly to chronic nocturnal intermittent hypoxia, specifically the oxidative desaturation index and oxy-haemoglobin saturation of <90%, replacement markers for hypoxia were found to be independent contributors to hypercholesterolemia and hypertriglyceridemia[1]. Others researchers argue that sleep fragmentation may also play a key role in dyslipidaemia in OSA, since the association between metabolic disorders and sleep loss, which could be caused by total sleep deprivation, chronic sleep restriction, or sleep fragmentation[2]. However, in a large general population sample one study[3] demonstrated the complaint of a sleep disturbance and chronic emotional stress are the primary predictors of short sleep duration reported by obese people. This detection and recognition of sleep issues should be part of the multidimensional treatment strategy for obesity and may lead to prevention of the increasing prevalence of obesity in modern societies.
For that reason result necessary to mention a randomized controlled investigation which determine if weight loss and/ or changes in apnea-hypopnea index (AHI) improve sleep architecture in overweight/ obese adults with type 2 diabetes (T2D) and obstructive sleep apnea (OSA)[4].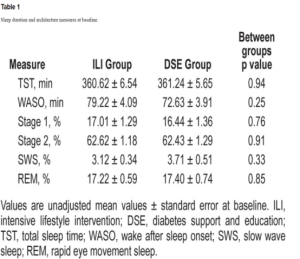
Methods: This was a randomized controlled trial including 264 overweight/obese adults with T2D and OSA. Participants were randomized to an intensive lifestyle intervention (ILI) or a diabetes and support education (DSE) control group. Measures included anthropometry, AHI, and sleep at baseline and year-1, year-2, and year-4 follow-ups.
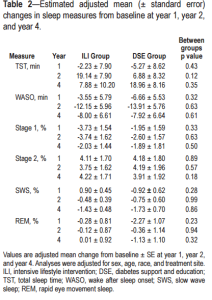
Results: Changes in sleep duration (total sleep time [TST]), continuity [wake after sleep onset (WASO)], and architecture stage 1, stage 2, slow wave sleep, and REM sleep) from baseline to year 1, 2, and 4 did not differ between ILI and DSE. Repeated-measure mixed-model analyses including data from baseline through year-4 for all participants demonstrated a significant positive association between AHI and stage 1 sleep (p < 0.001), and a significant negative association between AHI and stage 2 (p = 0.01) and REM sleep (p < 0.001), whereas changes in body weight had no relation to any sleep stages or TST. WASO had a significant positive association with change in body weight (p = 0.009).
Conclusions: Compared to control, the ILI did not induce significant changes in sleep across the 4-year follow-up. In participants overall, reduced AHI in overweight/obese adults with T2D and OSA was associated with decreased stage 1, and increased stage 2 and REM sleep. These sleep architecture changes are more strongly related to reductions in AHI than body weight, whereas WASO may be more influenced by weight than AHI.
[1] Chou, Y. T. et al. Hyperlipidaemia in patients with sleep-related breathing disorders: prevalence & risk factors. Indian J Med Res 131, 121–125 (2010).
[2] Qian, Y. et al. Independent Association between Sleep Fragmentation and Dyslipidemia in Patients with Obstructive Sleep Apnea. Sci. Rep. 6, 26089; doi: 10.1038/srep26089 (2016).
[3] A N Vgontzas, H-M Lin, M Papaliaga, S Calhoun, A Vela-Bueno, G P Chrousos and E O Bixler. Short sleep duration and obesity: the role of emotional stress and sleep disturbances
[4] Shechter A1, St-Onge MP1, Kuna ST2, Zammit G3, RoyChoudhury A1, Newman AB4, Millman RP5, Reboussin DM6, Wadden TA7, Jakicic JM4, Pi-Sunyer FX1, Wing RR5, Foster GD8; Sleep AHEAD Research Group of the Look AHEAD Research Group. Sleep architecture following a weight loss intervention in overweight and obese patients with obstructive sleep apnea and type 2 diabetes: relationship to apnea-hypopnea index. J Clin Sleep Med. 2014 Nov 15;10(11):1205-11. doi: 10.5664/jcsm.4202.


