21 Sep Diagnosis and treatment of severe eosinophilic asthma
Severe eosinophilic asthma (SEA) is a subphenotype of asthma that is not adequately defined in the current literature. The complex pathophysiological mechanisms that characterise SEA often result in patients becoming resistant to regular corticosteroid treatment with persistent increased airway inflammation as a result of elevated blood and airway eosinophil count. Increased inflammation demonstrated with SEA makes management for patients difficult with frequent and protracted exacerbations in ventilation often impacting on their overall quality of life.
Pathophysiology
Eosinophils found in the bronchioles and distal airway are generated through the “abnormal production of type 2 cytokines from T-helper 2 and innate lymphoid cells” (Buhl et al., 2017). Previously it was determined the development of eosinophils in the bronchioles was an allergic reaction driving an immune response that upregulated T-helper 2 cytokine production, a process which plays an integral role in the survival of eosinophils. The literature debated this and proposed that an eosinophilic inflammatory response in the airways corresponded with increases to innate lymphoid cells which are allergen-independent. This pathophysiological mechanism was more relative to SEA as insidious onset of the disease is more prevalent adult patients.
Diagnostic Pathway
Recent research has attempted to develop a pathway through diagnosis, treatment and management for SEA patients. Firstly, SEA needs to be distinguished from other asthma phenotypes in order for precise diagnosis. Symptoms will initially manifest as poor control using inhaled corticosteroid treatment with the frequent occurrence of severe exacerbations, but precise diagnosis of SEA in patients’ requires confirmation with elevated blood and sputum eosinophil counts. Performing eosinophil analysis on sputum is often impractical in clinical practice and can be supplemented with blood eosinophil measures and exhaled nitric oxide fraction (FeNO) to evaluate airway inflammation. This diagnostic model has been shown to improve the overall diagnostic accuracy eosinophilic respiratory diseases.
Treatment and Management
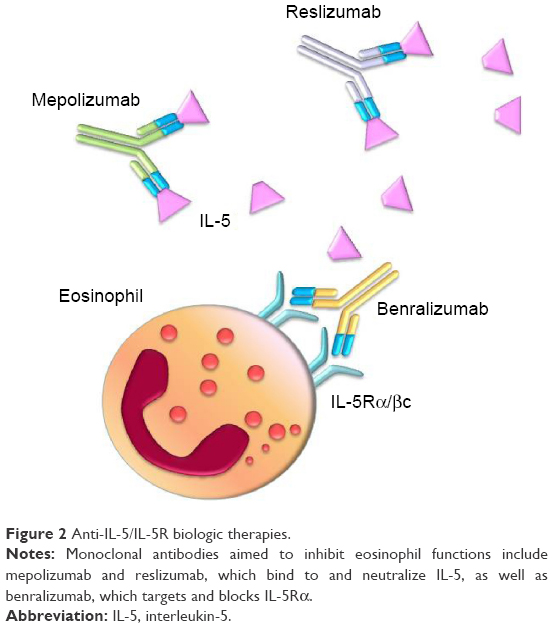
SEA patients are currently treated with anti-immunoglobulin E or anti-interleukin-5 therapies such as omalizumab and mepolizumab. These therapies of been approved for severe asthma but no treatment as such as been developed for the eosinophilic phenotype. Therefore managing treatment for SEA patients on biologic therapy requires frequent monitoring to identify responders and non-responders (Figure 1). As these current treatments are not curative, evaluating patient response is vital to ensure the efficacy of the anti-eosinophilic therapy and whether different or concurrent treatment is required.
Figure 1: From Buhl et al. (2017). Severe eosinophilic asthma: a roadmap to consensus. Eur Respir J; 49(1700634)
References
Buhl, R et al. (2017). Severe eosinophilic asthma: a roadmap to consensus. Eur Respir J; 49, 1700634 – 2017.
De Groot, J. C., ten Brinke, A., & Bel, E. H. D. (2015). Management of the patient with eosinophilic asthma: a new era begins. ERJ Open Research, 1(1), 00024–2015. http://doi.org/10.1183/23120541.00024-2015


