01 Feb Sleep and Eye Disorders
Optic Nerve Dysfunction in Obstructive Sleep Apnea: An Electrophysiological Study
(Liguori et al., 2016)
- The aim of this study was to evaluate the integrity of the visual system in patients affected by obstructive sleep apnea (OSA) by means of electroretinogram (ERG) and visual evoked potential (VEP).
Conclusion: Obstructive sleep apnea patients without medical comorbidities show alterations in visual evoked potentials consistent with subclinical optical nerve dysfunction, which may be provoked by hypoxia, acidosis, hypercapnia and airway obstruction. This report reinforces the importance of early identification and treatment of obstructive sleep apnea, which may prevent the occurrence or progression of optic nerve dysfunction.
Reference: Liguori, C., Palmieri, M., Pierantozzi, M., Cesareo, M., Romigi, A., Izzi, F., Marciani, M., Oliva, C., Mercuri, N. and Placidi, F. (2016). Optic Nerve Dysfunction in Obstructive Sleep Apnea: An Electrophysiological Study. SLEEP, 39(01), pp.19-23.
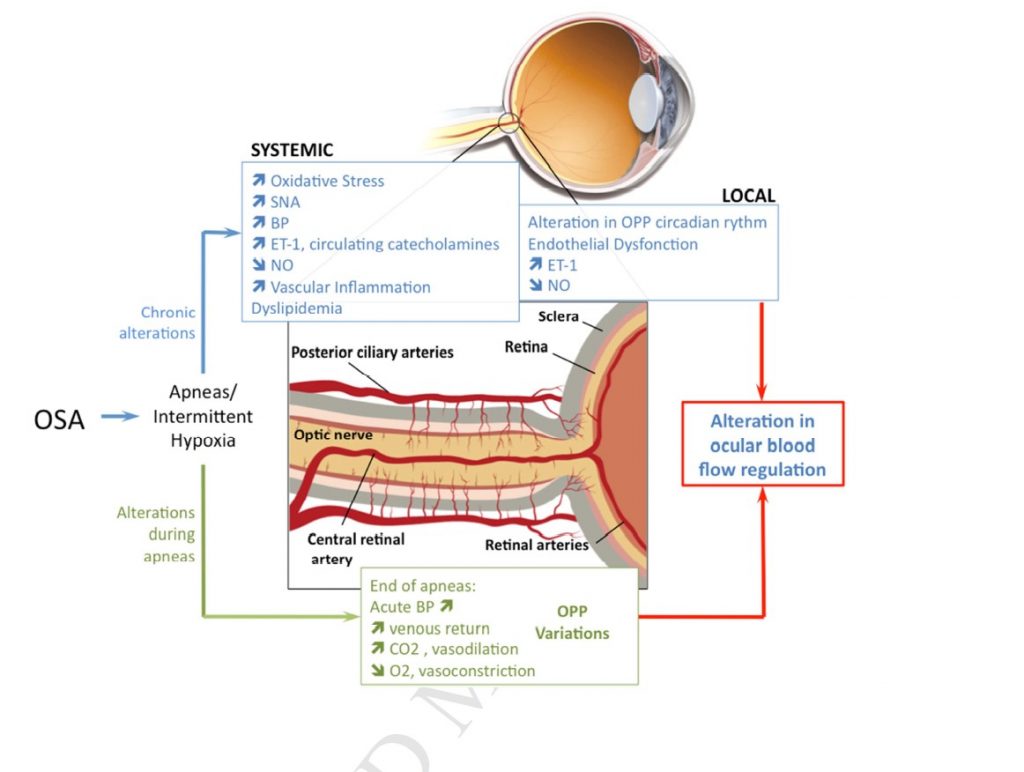
Diseases of the retina and the optic nerve associated with obstructive sleep apnea (Mentek et al., 2017)
- The object of the review article is to synthetize the possible vascular disorders of the retina and the optic nerve associated with sleep apnea patients and to discuss the underlying pathophysiological hypothesis.
- Main mechanisms involved in the ocular complications of OSA are related to intermittent hypoxia, sympathetic system activation, oxidant stress and deleterious effects of endothelin 1 (ET-1).
- The main evidence-based medicine data suggest that OSA should be screened in patients with ischemic optic neuropathy and diabetic retinopathy.
Conclusion: OSA is a frequent disease affecting 18% of the population over 50 years of age. OSA contributes to the appearance of hypertension, atherosclerosis, autonomic dysfunction, endothelial dysfunction, systemic inflammation and metabolic modification, which may interact with the vascular regulation of the eye. Many studies suggest that the supervision of retinopathy should be cautiously considered in diabetic OSA patients.
Reference: Mentek, M., Aptel, F., Godin-Ribuot, D., Tamisier, R., Pepin, J. and Chiquet, C. (2017). Diseases of the retina and the optic nerve associated with obstructive sleep apnea. Sleep Medicine Reviews.
Effects of Use of a Continuous Positive Airway Pressure Device on Glaucoma. (Ulusoy et al., 2015)
- The aim of the study was to investigate the prevalence of glaucoma in obstructive sleep apnoea syndrome (OSAS) and to determine the efficacy of the equipment used in the treatment of this disease.
- In this cross-sectional study, 38 patients with OSAS used continuous airway pressure (CPAP) and 32 OSAS patients with OSAS refused CPAP device treatment.
Conclusion: OSAS should be considered a significant risk factor for glaucoma. Eye tests may help to identify individuals with undiagnosed OSAS, and such testing of patients with diagnosed OSA may allow early detection of glaucoma and referral of such patients for CPAP therapy to prevent development of complications.
Reference: Ulusoy, S., Erden, M., Dinc, M., Yavuz, N., Caglar, E., Dalgic, A. and Erdogan, C. (2015). Effects of Use of a Continuous Positive Airway Pressure Device on Glaucoma. Medical Science Monitor, 21, pp.3415-3419.
FIGURE 1 Diagram illustrating pathophysiological hypotheses relating obstructive sleep apnea syndrome to retina and optic nerve disorders (Mentek et al., 2017)
SNA – Sympathetic nerve activity
BP – Blood pressure
ET-1 – Endothelin 1
NO – Nitric oxide
OPP – Ocular perfusion pressure