29 Jan Effect of changes in periodic limb movements under CPAP on adherence and long-term compliance in obstructive sleep apnea
For many people, who have been working in the field of Sleep medicine, the presence and emergence of PLMs after the CPAP initiation has been a total mystery.
The clinical significance of PLMs remains controversial; some characterize them as the motor symptom of restless legs syndrome although they can exist independently of any sensory symptom. By contrast, periodic leg movement disorder (PLMD) refers to the concomitant presence of PLMs and clinical sleep disturbances that cannot be explained by another primary sleep disorder, based on the International Classification of Sleep Disorders (ICSD-3). PLMD might induce sleep disturbances such as insomnia or excessive daytime sleepiness.
A newly published study has had as an aim to determine the predictors of Periodic leg movements (PLMs) change under CPAP and its impact on long-term adherence. They showed in their research that with CPAP treatment, OSA patients may show changes in their PLMs. PLMs can appear, increase, disappear, or remain unchanged despite the abolition of respiratory events. These changes under CPAP treatment appear to persist when the study of sleep is repeated several months later. All the research published about the topic has tried to explain this relationship, however it is still unclear. The researchers of this new investigation have assessed ferritin levels in OSA patients and the impact of emerging PLM on long-term adherence among patients with severe OSA being one of the first studies which include these important figures.
Given the comorbidity related to OSA and the potential additive effects of PLMs, the researchers believed that long-term adherence to CPAP treatment is crucial. The main goal was to assess the fate of PLMs in a group of OSA patients while on CPAP therapy, and determine if changes in PLM index could influence the long-term adherence and/or compliance to CPAP. Therefore, they analyzed all the PLMs, whether they were related to respiratory events or not. In this paper, they described their evolution under CPAP.
Material and Methods: Monocentric retrospective study. 160 patients referred to the sleep laboratory with a final diagnosis of severe OSA that required treatment with CPAP, according to the Belgian Social Security rules (an AHI >20 and movement arousal index (Ma): 30) on diagnostic full night polysomnography. All patients were offered a free CPAP trial of 3–5 days for habituation. A second polysomnography with CPAP was then performed to confirm if the treatment was effective.
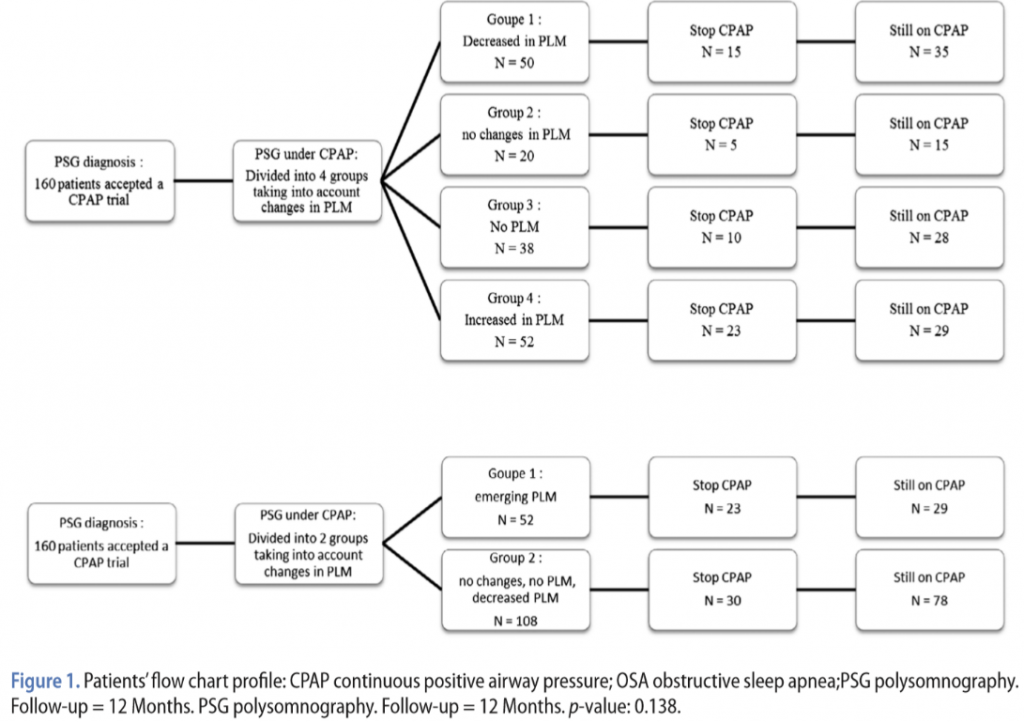
Two classifications of the cohort were established:
- Classification according to the change of the PLM index before and after CPAP treatment (see Table 1). We considered a variation in the PLMLs when they were superior to 5 h (see above). Four groups were defined:
- Group 1: reduction of the PLMI index: a decrease greater than 5 h.
- Group 2: no change in the PLM index.
- Group 3: absence of PLMs before and after CPAP treatment.
- Group 4: increase of the PLMI: an increase greater than 5 h.
- Classification according to emerging-PLM.
1-Group A: including patients who have increased their PLM index under treatment. (Group 4)
2- Group B: including patients who decrease their PLM, who do not have PLM, or who do not change their PLMI (Groups 1, 2, and 3).
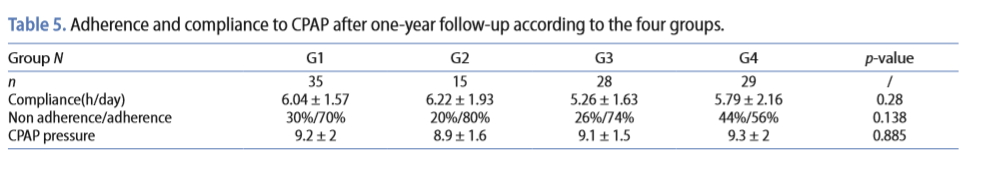
After one-year follow-up, they evaluated the CPAP adherence and compliance of patients into the different groups. Adherence was defined as the percentage of patients who continued the long-term treatment after receiving the CPAP device. Compliance was defined as the rate at which patients who successfully adhered to their treatment actually used it, defined as the mean number of hours of CPAP used per night according to the hour meter of the device.
Results: A total of 160 patients were recruited with a severe OSA. About 32.5% (52/160) patients had emerging PLM i.e. that appeared after the disappearance of respiratory events. By comparing patients with emerging-PLMs to others, we found that only the blood ferritin level was significantly different between groups. Moreover, after one-year follow-up, a significant difference in adherence and long-term compliance was observed between patients without PLM at both screening and CPAP polysomnographies or emerging PLM at the second study (56%) vs. patients with baseline PLM, whether PLM remained stable or decreased under CPAP treatment (75%) (p-value 0.028). Serum ferritin and presence of diabetes mellitus predicted the evolution of PLM observed. Patients with low ferritin levels demonstrated an increase of PLM after initiation of nasal CPAP treatment.
Conclusion: The emergence of PLM negatively impacts long-term adherence to nasal CPAP treatment in OSA. Blood ferritin level is a predictor of the evolution of PLM under CPAP therapy.
References:
Gimbada B. Mwenge, Ihsan Rougui & Daniel Rodenstein (2018) Effect of changes in periodic limb movements under cpap on adherence and long term compliance in obstructive sleep apnea, Acta Clinica Belgica, 73:3, 191-198, DOI: 10.1080/17843286.2017.1405137. Available online: https://doi.org/10.1080/17843286.2017.1405137