
29 Oct Case study: The importance of Complex Pulmonary Function Test versus Spirometry alone
Posted at 05:35h
in Medical Newsletter
An 84-year-old never-smoker (PHx passive smoke exposure) presented with mild shortness of breath.
- Mild SOB, increasing last 3/12
- No reported cough or wheeze
- No reported upper airway dysfunction (Rhinitis/Sinusitis)
- No SABA/SAMA/LABA/LAMA/ICS usage
- Rheumatoid Arthritis with long-term Methotrexate use.
Lung Function Test Results as follows: 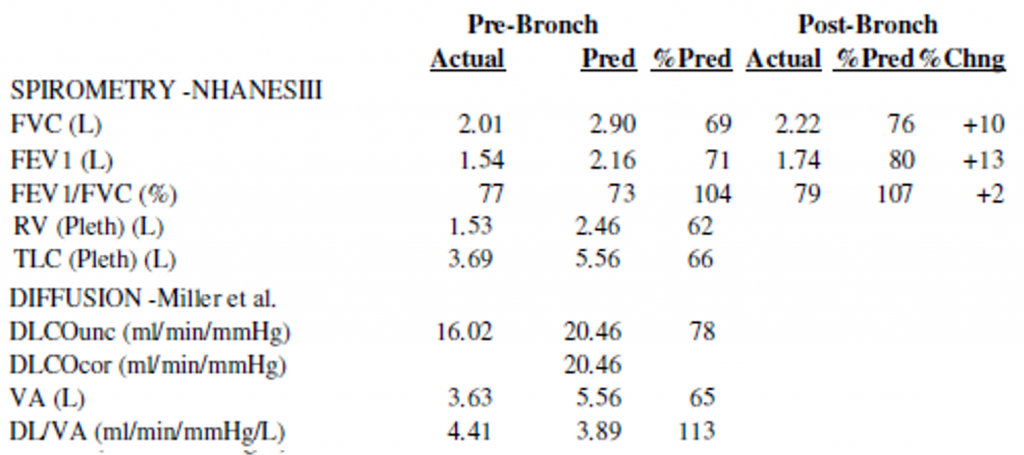
Test Findings:
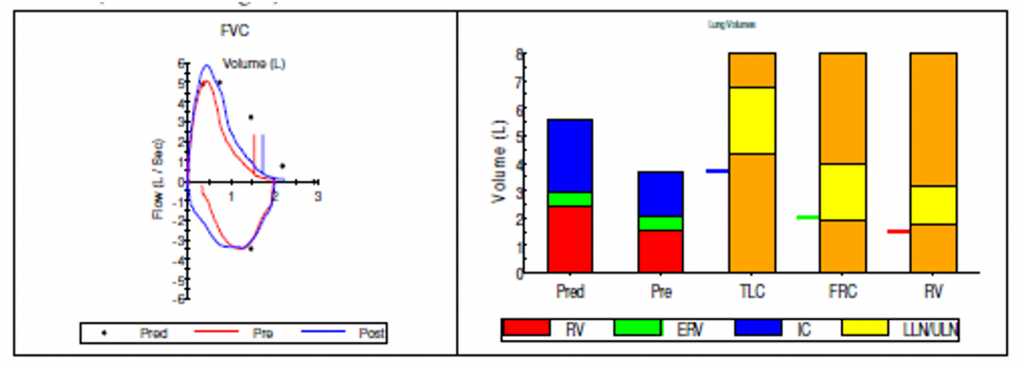
- Spirometry indicates normal FEV1/FVC ratio due to both parameters being equally reduced.
- Many interpretation algorithms may interpret this spirometry as purely obstructive in nature. Furthermore, post-BD spirometry indicated positive acute response to bronchodilator, consistent with reversible small airways disease.
- However, further testing indicates the patient had a reduction in Total Lung Volume (TLC), Residual Volume (RV), and Alveolar Volume (VA).
- A reduction in uncorrected gas diffusion (DLCOuncor) was due to reduction in TLC, however KCO corrected for VA.
Learning points:
- The lung volume and gas diffusion results give context to the spirometry result.
- These findings confirm the patient has a mixed ventilatory response, consistent with both obstructive and restrictive ventilatory impairment
- The obstructive component is consistent with asthma whilst the restrictive impairment may be associated with long-term methotrexate use.

