
26 Jul Sleep-disordered breathing during pregnancy
Maternal morbidity
The Sleep Disordered Breathing Sub-study of the Nulliparous Pregnancy Outcomes Study was a multicenter, prospective cohort study designed to estimate whether SDB during pregnancy is a risk factor for development of hypertensive disorders of pregnancy and gestational diabetes mellitus (GDM).
In early and mid-pregnancy, the adjusted odds ratio for preeclampsia when SDB was present was 1.94 (95% CI 1.07–3.51) and 1.95 (95% CI 1.18–3.23), and for GDM was 3.47 (95% CI 1.95–6.19) and 2.79 (95% CI 1.63–4.77). These results support findings from prior smaller cross-sectional and observational studies. Even after controlling for obesity, OSA is also associated with an increased risk of cardiomyopathy (OR, 9.0; 95% CI, 7.5-10.9), pulmonary embolism (OR, 4.5; 95% CI, 2.3-8.9) and in-hospital mortality (OR 5.1 95% CI, 2.4-11.5).
Neonatal morbidity
The adverse fetal and neonatal consequences of sleep apnea in pregnancy are less well delineated. Maternal OSA is associated with a 1.5- to 2-fold increased frequency of low birth weight and small-for-gestational-age infants, both in high-risk women and in an otherwise healthy non-obese cohort. These infants are also more likely to have preterm delivery and neonatal intensive care unit admission (despite similar gestational age at delivery). One study following 74 mom baby pairs 24% of which had OSA noted no difference in general motor scores but an increased frequency of low social development scores in neonates of moms with OSA (64% vs. 25%, P = .036) at age 12 months. There are no studies that indicate an increased risk of fetal death or miscarriage in association with sleep apnea.
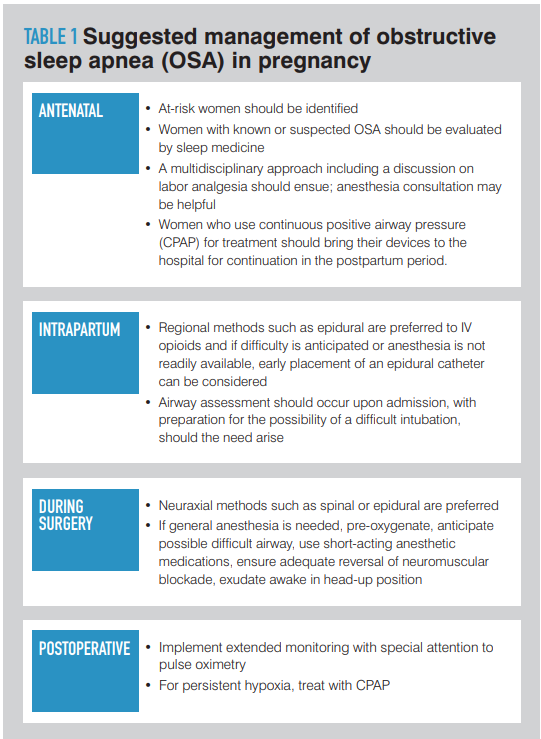
Table 1 shows the suggested management of OSA in pregnant women.
References
- Louis, Judette,M.D., M.P.H., & Street, L., M.D. (2018). Obstructive sleep apnea in pregnancy-what you need to know. Contemporary OB/GYN, 63(2), 18-20,22. Retrieved from https://search-proquest-com.ezproxy.unal.edu.co/docview/2025304964?accountid=150292

