26 Jun The early diagnosis of Restless legs syndrome (RLS) in primary care
The early diagnosis of Restless legs syndrome (RLS) in primary care
This article is primarily based on a report that details the considerations for Restless legs syndrome (RLS) diagnosis and management that were made during a European Restless Legs Syndrome Study Group (EURLSSG)-sponsored task force, consisting of experts and primary care practitioners. The task force pursued to develop a better understanding of barriers to diagnosis in primary care practice and overcome these barriers with diagnostic and treatment algorithms [1].
In order for RLS to be appropriately managed from primary care upwards, it is therefore necessary to provide GPs with both diagnostic and treatment guidelines.
To begin with, it is important to define what Restless legs syndrome (RLS) is. The RSL is a neurological disorder characterised by an irresistible urge to move the legs especially at rest. Symptoms worsen in the evening and night and improve with activity such as walking. RLS may be secondary to, or exacerbated by, a number of conditions that include iron deficiency, pregnancy, end stage renal disease (ESRD), diabetes and rheumatoid arthritis, or with neurological disorders such as peripheral neuropathy.
Why it is so important?.
As a consequence of sleep disruption and the inability to remain still (including during the daytime, the symptoms of RLS can severely impact on activities of daily living.
The main consequences of severe RLS are:
- Sleep disruption: RLS is the sleep disorder which causes the greatest chronic loss of sleep. Sleep loss by itself causes daytime drowsiness, difficulties concentrating, loss of performance and negatively impacts mood.
- Difficulties resting and remaining still: this happens predominantly in the evening and at night, but also at other times during the day. Consequently patients have difficulties with work, travelling and social events.
They have identified some barriers to diagnosis within the report that include the presentation of symptoms, the language used to describe them, the actual term “restless legs syndrome” and difficulties in the differential diagnosis of RLS.
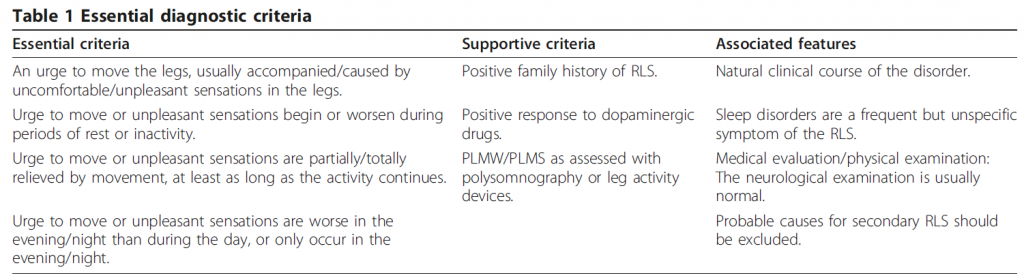
The diagnosis of RLS
[1] © 2011 Garcia-Borreguero et al; licensee BioMed Central Ltd. Algorithms for the diagnosis and treatment of restless legs syndrome in primary care. BMC Neurology 2011, 11:28 http://www.biomedcentral.com/1471-2377/11/28
Potential barriers to diagnosis
Presentation of symptoms
RSL does not present as a motor-sensitive problem, but through symptoms such as disturbed sleep pain or unspecific increased motor activity. The reason that sleep disturbance is often the reason for consultation is because the circadian pattern of RLS causes difficulty in falling asleep, getting back to sleep [23], and can cause awakenings during the night due to the discomfort in the limbs [26]. Patients’ quality of life can also be affected and chronic disruption of sleep or reduced duration of total sleep time can lead to depression, anxiety, cognitive and social dysfunction
The term “restless legs syndrome”
A major barrier to diagnosing RLS is the language patients use to describe their symptoms (see Table 2), as well as cultural differences that appear when RLS sufferers describe these symptoms. For example, a description of symptoms as resembling “water moving in my legs” does not confer the seriousness and credibility of symptoms.
The problem with the term “restless legs syndrome” is that it is a term that is confusing, because it gives the impression that RLS is a lifestyle disorder as opposed to a nosological entity with a genetic basis.
Differential diagnosis and mimics
The diagnosis of RLS necessitates that the physician is aware of the disorder and its variety of symptoms. When there is a lack of awareness about what exactly RLS is, then the probability of misdiagnosis is more likely. This is especially the case with RLS mimics, which meet the essential diagnostic criteria but do not constitute RLS.
Important mimics include peripheral neuropathy, cramps, positional discomfort, akathisia and anxiety disorders.
RLS also needs to be differentiated from other conditions that can also coexist with it such as peripheral neuropathy, lower limb pain conditions of different origin, parkinsonism with sensory symptoms or motor fluctuations with dyskinesia etc.
The high prevalence of concomitant RLS in the Parkinson’s disease population may reflect the medication effect; however there may also be mimics or overlap of some PD symptoms with RLS.
RLS is a common condition that can present frequently in primary care setting. Due to the important consequences on quality of life, and the availability of treatment, it is important to identify such cases in primary care. RLS is probably one of the most easily manageable medical causes of insomnia, and thus, it is important that GPs become familiar with this disorder, it’s diagnosis and management. Given the impact of RLS on quality of life and the marked therapeutic efficacy of current treatments in improving these symptoms, its early identification and treatment is highly relevant.
References
[1] Garcia-Borreguero et al; licensee BioMed Central Ltd. Algorithms for the diagnosis and treatment ofrestless legs syndrome in primary care. BMC Neurology 2011, 11:28 http://www.biomedcentral.com/1471-2377/11/28