06 Dec Treatment-Emergent Central Sleep Apnoea (Complex Sleep Apnoea)
Abstract:
Treatment-emergent central sleep apnoea (TECSA) is a distinct form of sleep-disordered breathing characterized by the development of central sleep apnoea during the initiation of positive airway pressure (PAP) therapy in patients with obstructive sleep apnoea. The exact mechanisms of TECSA are not clearly known; however, several theories have been proposed. Usually, TECSA is transient and self-limited, and disappears after continued PAP use. Nevertheless, patients with persistent TECSA have lower adherence to PAP therapy and are more likely to terminate therapy. Close follow up is necessary to assure that the emergent central events disappear with continued therapy. In patients with persistent TECSA, more advanced algorithms such as adaptive servo-ventilation have been shown to be very effective.
Meaning:
Treatment-emergent central sleep apnoea (TECSA) is otherwise known as complex sleep apnoea. Nevertheless, it more accurate to call it positive airway pressure (PAP)-emergent central sleep apnoea (CSA) or TECSA. In 2017, a European Respiratory Society Task Force identified nocturnal central breathing disturbances and recognized this disorder as TECSA. This term refers to the development of CSA during PAP therapy in the form of continuous positive airway pressure (CPAP), bi-level positive airway pressure (BPAP), or auto titrating PAP as treatment of obstructive sleep apnoea (OSA). It can be defined as the appearance of repetitive CSA in patients with OSA after the initiation of PAP.
Pathophysiology
Treatment-emergent central sleep apnoea is basically central sleep apnoea (CSA). CSA is characterized by cessation of airflow without respiratory effort.
Pathophysiology of CSA
During sleep, the wakefulness drive to breathe is no longer working, and breathing is totally under metabolic control. Additionally, the hypercapnic and hypoxic drives are reduced, and there is also increased upper airway resistance. CSA can result secondary to unstable breathing caused by high loop gain, or secondary to a reduced output from the central neurons. Therefore, high loop gain results in hyperventilation, and a lower PaCO2 level below the apnoeic threshold. When PaCO2 drops below the apnoeic threshold, ventilation will cease and an apnoea will occur and last until the PaCO2 increases above the threshold.
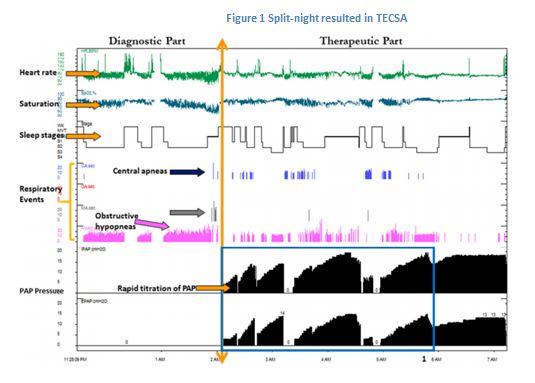
TECSA may occur at any PAP setting. In general, PAP therapy settings in patients demonstrating TECSA are not much different from those in patients without central apnoeas. Nevertheless, high PAP pressure, use of BPAP or rapid titration may lead to mask leaks and pressure intolerance, which could lead to sleep fragmentation and central apnoeas.
The exact cause of this type of CSA is not known. However, several hypotheses have been proposed.
- One theory is that the application of PAP results in the relief of upper airway obstruction, which causes an increase in carbon dioxide (CO2) washout. In other words, upper airway resistance can weaken the ventilatory control system, and hence reduce the efficiency of CO2 excretion.
- Another proposed mechanism is that significant mask leak or mouth breathing (with nasal mask) may develop at high PAP levels resulting in washout of CO2 from the anatomical dead space, which results in a drop in CO2 below the apnoea threshold.
- A third possibility is that PAP initiation may worsen sleep quality causing frequent transitions from sleep to wake to sleep states, resulting in frequent arousals. The resulting arousals can stimulate the ventilatory response, which reduces PaCO2 below the CO2 apnoea threshold, yielding CSA during subsequent sleep. However, this associated CO2 fluctuations also tend to resolve over time as patients adjust to the interface and the application of PAP therapy.
- When BPAP is used, inspiratory PAP can lead to augmented tidal volumes, which decrease PaCO2. If the PaCO2 falls below the CO2 apnoea threshold, CSA may follow.
Treatment
In most TECSA cases, apnoea events during initial PAP titration are self-limited and disappear overtime. A follow-up is needed to make sure that the emergent central events disappear with continued therapy. This can be done through tracking the PAP stored data and close clinical review.
References:
- BaHammam, Ahmed S. Treatment-Emergent Central Sleep Apnea (Complex Sleep Apnea). Sleep Vigilance (2017). DOI 10.1007/s41782-017-0015-8
- International Classification of Sleep Disorders (ICSD-3). 3rd ed. Chicago: American Academy of Sleep Medicine; 2014.
- Randerath W, Verbraecken J, Andreas S, Arzt M, Bloch KE, Brack T, et al. Definition, discrimination, diagnosis and treatment of central breathing disturbances during sleep. Eur Respir J. 2017;49(1):1600959. doi:10.1183/13993003.00959- 2016. Quoted by BaHammam. A. S
- Castriotta RJ, Majid R. Complex sleep apnea. Sleep Med Clin. 2013;8:463–75. Quoted by BaHammam. A. S
- Berssenbrugge A, Dempsey J, Iber C, Skatrud J, Wilson P. Mechanisms of hypoxia-induced periodic breathing during sleep in humans. J Physiol. 1983;343:507–24. Quoted by BaHammam. A. SMalhotra A, Bertisch S, Wellman A. Complex sleep apnea: it isn’t really a disease. J Clin Sleep Med. 2008;4(5):406–8. Quoted by BaHammam. A. S


