26 Oct STOP-BANG & The Epworth Sleepiness Scale
For Referrals containing these questionnaires, follow this link: http://thoracicandsleep.com.au/referrals-online-referral/
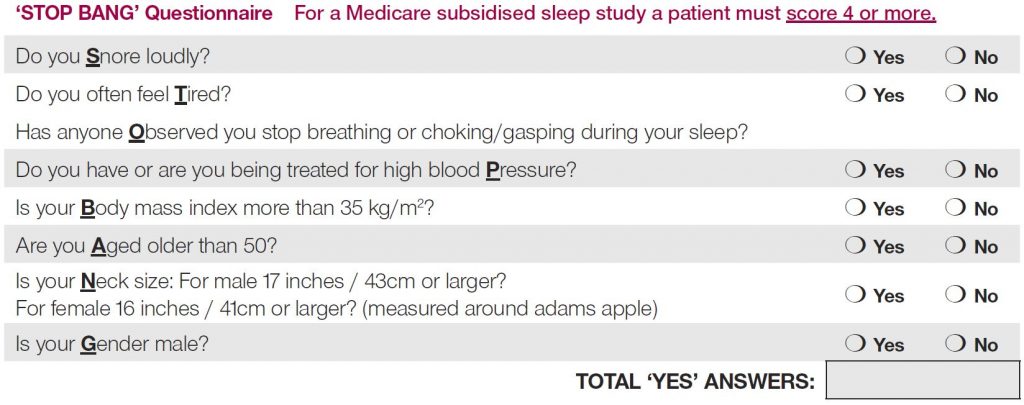
STOP-BANG
The STOP-BANG screening tool has become a well-known and used screening tool for identifying obstructive sleep apnoea. As of 1st November 2018 MBS items for thoracic medicine are changing, all direct GP referrals for either home or in-lab sleep studies will need a positive score of 4 or more on the STOP BANG (or equivalent) questionnaire AND a positive score of at least 8 in the Epworth Sleepiness Score.
The STOP BANG questionnaire was originally developed as a fast simple way of identifying patients at risk of having OSA prior to surgery, due to the complications and adverse events associated with untreated OSA during surgery.
The benefit of the STOP-BANG is that it’s a simple questionnaire which can be quickly completed. It is an acronym for a series of questions, answering yes to one of these questions will score a point while a no will score not.
A low STOP BANG score does not necessarily rule out a sleep related breathing disorder.
SCORING
For general population
OSA – Low Risk: Yes to 0 – 2 questions
OSA – Intermediate Risk: Yes to 3 – 4 questions
OSA – High Risk: Yes to 5 – 8 questions
Generally a score 0-2 indicates a low probability of OSA, 7-8 is a high risk and 3> is considered suggestive of OSA.
As a rule, the sensitivity for the test is quite strong for identifying moderate – severe OSA with a score of 3 or more, meaning a high number of patients with disease will be accurately detected. The specificity however is relatively low. Hence the need for further testing.
Epworth Sleepiness Scale
Many sleep disorders are characterized by patients suffering from excessive daytime sleepiness. In order to help assess a patient’s general level of sleepiness, and determine if sleep disorders could be the cause of their problems, Dr Murray Johns of the Epworth Hospital in Melbourne created a screening tool called the Epworth Sleepiness Scale (ESS).
The ESS has become the standard assessment tool for symptoms of sleepiness because it is a very quick questionnaire to complete and it gives a generalized level of a person’s average sleepiness. The ESS is not a diagnostic tool in itself however. It is primarily used by physicians and sleep medicine professionals to determine whether a patient should schedule a sleep study to diagnose, or rule out sleep disorders that may be affecting their everyday sleep.
As of 1st November 2018 MBS items for thoracic medicine are changing, all direct GP referrals for either home or in-lab sleep studies will need a positive score of at least 8 in the Epworth Sleepiness Score AND a positive score of 4 or more on the STOP BANG (or equivalent) questionnaire.
The ESS is a self-administered questionnaire with 8 questions. Respondents are asked to rate, on a 4-point scale (0-3), their usual chances of dozing off or falling asleep while engaged in eight different activities. Most people engage in those activities at least occasionally, although not necessarily every day.
Likelihood of having a sleep disorder is ranked on a scale of 0-24 after all questions have been answered, and the total points of “chances of dozing” are added to produce a single number.
- 0-7: Unlikely that patient is abnormally sleepy
- 8-9: Patient has an average amount of daytime sleepiness
- 10-15: Patient may be excessively sleepy depending on the situation. Patient may want to consider seeking medical treatment
- 16-24: Patient is excessively sleepy and should consider seeking medical attention.
The ESS is used primarily to validate symptoms of sleep apnoea, narcolepsy, and idiopathic hypersomnia. All of which list excessive daytime sleepiness as a primary symptom.
For more information on the changes to Medicare item numbers for Thoracic and Sleep Medicine refer to the links below: http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Factsheet-SleepDisorders
https://www1.racgp.org.au/newsGP/Professional/Changes-to-the-Medicare-Benefits-Schedule-What-GPs